Abstract
Background: In recent years, there has been a large amount of studies about the efficacy and safety of vernakalant or RSD1235, an antiarrhythmic agent, in treating the atrial fibrillation (AF). This study was designed to assess the efficacy and safety of vernakalant in the treatment of AF.
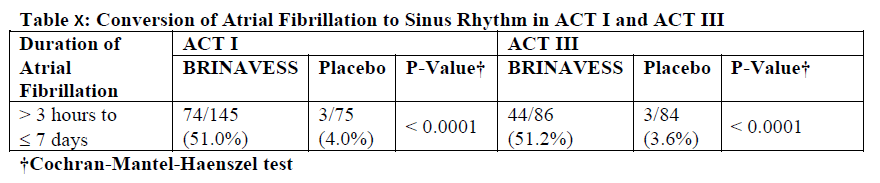
Results: A total of 5 randomized controlled trials (RCTs) (n= 1153) met our inclusion criteria. Vernakalant was superior in achieving sinus rhythm (SR) for AF comparing to placebo or alternative anti-arrhythmic agents (relative risk [RR] = 11.56, 95% Confidence Interval [CI] = 7.12 – 18.75). There was no heterogeneity among the trials (X2 =0.59, P = 0.96). In analysing the adverse effects of cardiac origin, there was no significant difference between the two groups (RR= 0.90, 95% CI = 0.52 – 1.57). Methods: The Cochrane library, Pubmed NCBI, EMBASE and MEDLINE were systematically searched to identify all interventional trials of vernakalant with placebo or other antiarrhythmic drug in converting AF to SR. The primary outcome was rate of converting to SR, and the secondary outcome was the rate of adverse effects of cardiac origin due to vernakalant and the placebo or amiodarone. Meta-analyses were carried out using Mantel-Haenszel fixed-effects or random effects models and heterogeneity was by the X2 test.
Conclusion: In the conversion of AF to SR, vernakalant is highly effective without obviously raised side effects. Owing to only one study comparing vernakalant with amiodarone included in this study, the efficacy of vernakalant comparing to other antiarrhythmic agents needing more well-designed double-blinded RCTs to be confirmed.
לקריאת המאמר: